Many of us have either experienced or know of someone who has experienced the notoriously painful strike in the bunion joint of the big toe by gout, usually at night. Gout results from excess uric acid, which forms sharp, needle-like mineral crystals in the joints, causing inflammation and pain.
Gout has for centuries been associated with high levels of uric acid. From the 1960’s onwards the numbers of gout patients in the Western World have surged. However, during the last decade or so researcher have found that uric acid isn’t just about gout and that the surge in gout patients parallel the increased consumption of the ingredient that causes high levels of uric acid, namely the fructose in sugar.
During the 1960’s an increased awareness of the perceived danger of fat in food has led to a swing to low-fat or fat-free foodstuff. (Without distinguishing between “good fats” and “bad fats”.) To make the lower-fat foods more palatable, manufacturers added more sugar. The latest research has increasingly linked sugar-rich diets to various health problems, with high levels of uric acid shown to be a major instigator
At the forefront of enlightening the medical community and the public at large about the dire effects of uric acid, is Dr David Perlmutter, who not only do regular talk shows on the subject, but also published a book on this topic in 2022, called DROP ACID.
How is uric acid linked to sugar?
A single molecule of sugar consists of equal amounts of glucose and fructose, which gets separated early during the digestive process in the small intestine. Fructose is quickly absorbed into the bloodstream and ends up in the liver.
Fructose metabolism in liver cells uses the energy molecules ATP (adenosine triphosphate, manufactured in the body’s cells using glucose as fuel), but in an unregulated way, rapidly depleting energy resources. During this interaction, ATP gets converted into the molecule AMP (adenosine monophosphate) as part of a complicated chain of chemical events and ultimately generates uric acid as an end-product. High levels of fructose can deplete 40% to 50% of ATP in liver cells.
While ATP ends up as uric acid during metabolism in the liver, the metabolized fructose in the liver is converted into fat and stored in the liver and fat cells in the body.
Other sources and instigators of high uric acid:
According to Dr. Perlmutter, uric acid mainly comes from three sources, namely fructose, as seen above, purines, and alcohol.
Purines are a class of chemicals that are found in all living cells and these organic substances are used to help form both DNA and RNA, which are the body’s core genetic material in cells. The body’s cells are continuously in a state of death and renewal. With normal cell turnover, breakdown of DNA and RNA occurs. When genetic material such as damaged, dying, or dead cells in the body are degraded, purine bases are released. Many are reused, but some are further metabolized to form uric acid.
About two-thirds of purines are produced naturally by the body and found inside cells, while the rest of the purines in the body come from foods such as red meat (beef, lamb, pork, liver, and kidney), certain seafoods (anchovies, sardines, and herring), multigrain breads, some vegetables and legumes. Beer especially is very high in purines due to its yeast content.
Purines at normal levels are not harmful, however excessive amounts from a high intake of purine-rich foods result in the body being unable to process all of it, leading to high levels of uric acid build up in the bloodstream.
Alcohol has been described as “fructose with a buzz”, as alcohol is metabolized similarly to fructose in the liver, as it also converts ATP to AMP, leading to the formation of uric acid. Alcohol further increases the formation of uric acid mainly in three ways:
- Certain types of alcohol can be a source of purines, for example beer is high in purines.
- The kidneys switch to excreting alcohol, when they could have excreted uric acid, which leaves more uric acid to circulate in the bloodstream.
- Alcohol increases the metabolism of nucleotides, which are additional sources of purines that can form uric acid. Nucleotides are organic molecules that are the basic building blocks of DNA, RNA, AMP and ATP.
As beer is made with brewer’s yeast, it is high in purines and contains alcohol, this double effect resulting in a higher production of uric acid than from liquor. Moderate wine drinking would not affect uric acid levels.
Other contributors to high levels of uric acid:
Salt. There is mounting evidence that a high intake of salt can trigger the production of uric acid by stimulating the conversion of glucose into fructose, through the activation of an enzyme called aldose reductase (Polyol pathway). Salt is a well-known contributor to high blood pressure and a high intake of salt may also predict the development of diabetes and nonalcoholic fatty liver disease.
Sleep. Just like Eskom, where the lack of proper maintenance leads to equipment failure at power stations, the lack of maintenance being done in the body due to lack of proper sleep leads to a wide range of health problems, as it affects many critical biological processes. Studies have correlated poor-quality, short-duration sleep with high levels of uric acid, proving that a good night’s sleep helps to keep uric acid levels in check.
Medication: Certain medications can increase uric acid, by having effects such as increasing the reabsorption of uric acid, decreasing the secretion of uric acid, or increasing the production of purines. For example, chemotherapy drugs liberate purines while destroying cancer cells, resulting in increased uric acid. Other drugs that may raise uric acid levels include aspirin in doses of 60-300 mg daily; testosterone replacement drugs; anticonvulsive drugs; blood thinners; Viagra; proton-pump inhibitors for acid reflux; immunosuppressants; Parkinson’s medication; white blood cell count treatments; water pills; and beta blockers. Xylitol, although a natural sugar, has been found to increase urate levels by stimulating the breakdown of purines in the body.
Sitting: A Korean research project in 2019 found that people who spent ten or more hours per day sitting, with too little exercise, were more inclined to have high levels of uric acid.
Health conditions linked to elevated uric acid:
Metabolic syndrome: Several metabolic risk factors are grouped under the umbrella term metabolic syndrome. Together they raise the risk of coronary heart disease, diabetes, stroke, sleep apnea, liver and kidney disease, cancer, dementia, and Alzheimer’s disease. You may be at risk of being diagnosed with metabolic syndrome if you have three or more of the following conditions:
- A large waistline (abdominal obesity).
- High blood pressure.
- High blood sugar levels.
- High blood levels of triglycerides
- Low levels of the “good” HDL cholesterol.
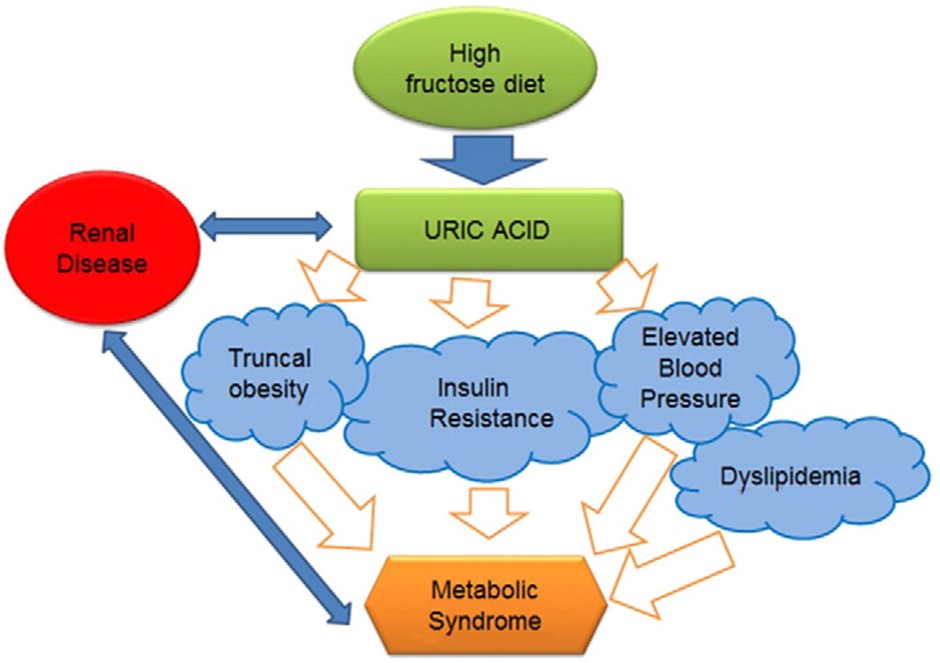
The high consumption of fructose is one of the main causes of metabolic syndrome and the resulting high uric acid is not only one of the markers of metabolic syndrome, but lately also regarded as a contributory causal factor for metabolic syndrome, as it may precede the development of these metabolic conditions.
Manifestations of metabolic syndrome:
- Cardiovascular disease: Studies have indicated that high levels of uric acid are an independent risk factor for the development of cardiovascular disease, for instance patients with gout experience more frequent coronary heart disease and have a two-fold greater evidence of angina pectoris (chest pain and discomfort). The prevalence of calcium buildup in the walls of arteries that supply oxygen rich blood to the heart, a condition called coronary calcification, which results in hardening of arterial walls, corresponds with higher uric acid levels in the bloodstream. Studies found that increase uric acid level is a potent risk factor for atherosclerosis (hardening and narrowing of arteries due to cholesterol plaques lining the arteries over time) and endothelial dysfunction (impaired functioning of the inner lining of arteries). Uric acid is also known to directly or indirectly induce remodeling of vascular structures. However, the precise mechanism by which uric acid induces cardiovascular disease has not been clearly defined.
- Hypertension: High blood pressure increases the risk of cardiovascular disease and mortality. Studies have revealed that hyperuricemia has also been identified as a risk factor for hypertension, apart from the more well-known factors that predict the onset of hypertension, such as dietary salt intake, alcohol intake, body weight, glucose intolerance, and increased arterial stiffness. Higher uric acid levels, although still within the normal range, increase the risk of hypertension. The strong relationship between high levels of uric acid and hypertension is deemed to be largely due to its lowering effect on nitric oxide levels, a powerful regulatory molecule in vasodilation.
- Insulin resistance and diabetes type 2: Elevated levels of uric acid in the bloodstream usually precedes the development of both insulin resistance and diabetes type 2, and high levels are a strong predicter of and risk factor for diabetes. Hyperuricemia may play a role in inducing or worsening insulin resistance. Studies found a higher incidence of insulin resistance in patients with gout than in the general population, as well as finding that decreased uric acid clearance from the body was inversely proportional to increased insulin resistance, resulting in increased uric acid levels in the bloodstream. Insulin requires nitric oxide to move out of blood vessels to gain entry into the body cells, which helps to keep blood sugar under control. This process is threatened by uric acid and studies found evidence that fructose-induced hyperuricemia leads to insulin resistance.
- Non-alcoholic fatty liver disease: Several studies have linked high levels of uric acid in the blood stream with non-alcoholic fatty liver disease, which occurs through several intricate chemical processes in the liver, some of which can cause inflammation, resulting in damaged liver cells and creating fibrosis or scarring of the liver. Uric acid also directly increases production of fat in the liver cells.
- Immune system: High levels of uric acid is a danger signal which alerts the immune system to trigger immune responses, which may result in systemic inflammation, an inflammatory state that affects the whole body. High levels of uric acid also cause more pro-inflammatory responses in the gut microbiome, increasing gut permeability. Inflammation is regarded as the centerpiece of the damage done by uric acid.
- Brain health: Increased levels of inflammation due to hyperuricemia is one of the multiple inputs for developing dementia and Alzheimer’s disease. Another input is the way uric acid compromises the way insulin works throughout the body, including the brain. A 12-year study concluded in 2018, in which uric acid levels and neurocognitive testing were done every two years, found that those individuals with high uric acid levels had an 80% increased risk for being diagnosed with dementia, with a 55% increased risk of Alzheimer’s disease.
Studies have shown that the components of metabolic syndrome are raised with increasing concentrations of uric acid in the bloodstream, while recent studies have shown the potential development of metabolic syndrome being mediated by fructose-induced hyperuricemia. There is also a higher prevalence of metabolic syndrome in patients with gout, compared to the general population. More studies are however needed to determine the exact role of hyperuricemia in the development of metabolic syndrome.
Various other health conditions are also linked to elevated levels of uric acid:
Psoriasis: This chronic inflammatory skin disorder is immune-related and many (about 25%) of these patients also suffer from psoriatic arthritis, a joint disease. Scientists have recently linked high levels of uric acid to this disorder, due to the rapid turnover of skin cells and systemic inflammation associated with this condition.
Kidneys: Chronic kidney disease and renal insufficiency means the kidneys lack in capacity for the filtering and excretion of waste products, leading to a build-up of uric acid in the bloodstream.
Thyroid: Insufficient levels of thyroid hormones, a condition called hypothyroidism, can negatively impact uric acid excretion and lead to an increase in uric acid levels in the bloodstream. The other extreme, elevated thyroid function, called hyperthyroidism, can lead to the breakdown of tissues, resulting in the release of purines, with increased levels of uric acid.
Gout and kidney stones: With serum urate levels above 0,42mmol/l being the limit of urate solubility, higher concentrations of uric acid can coalesce into crystals, which can settle in joints and cause inflammation, resulting in a very painful form of arthritis typified by pain, swelling, and loss of joint motion, called gout. These crystals can also settle in the kidneys and result in the forming of kidney stones. Uric acid accounts for about 7% of all kidney stones.
Interestingly, not only pH but also temperature plays a role in urate solubility. As the toes are the coldest part of the body, gout usually first manifests in the joints of the big toes.
Gout symptoms usually come on suddenly and initially affects a single joint, often the joint where the big toe meets the foot. It is called a gout attack for good reason, as the affected joint becomes red, swollen, hot, and very painful. Other common sites are joints in the many small bones in the foot, the knees, and the ankles. People with osteoarthritis often experience their gout attacks in the joints of the fingers.
Gout can be accurately diagnosed by medical practitioners, as the uric acid crystals can be seen in the fluid taken from a swollen joint or seen in imaging of the bones and joints with ultrasound, X-rays, or CAT scans.
Many people with high levels of uric acid can remain asymptomatic and never develop gout or any other symptoms.
Preventing high levels of uric acid:
It is quite possible to limit the sources of uric acid in foods. Drinking at least 8 cups of water daily can help to flush uric acid out through the kidneys.
- Foods high in fructose: Sweetened food and beverages are the major sources of high levels of fructose, resulting in high levels of uric acid and fat in the body. Sugar consists of glucose and fructose molecules bound together in equal amounts. The separation of glucose and fructose takes place immediately during digestion in the small intestine. While glucose is the currency of energy in the body, fructose is the currency of energy storage. Glucose fuels every cell in the body and levels are constantly controlled in the body, mainly through the hormone, insulin. During digestion, fructose is quickly absorbed into the bloodstream and ends up in the liver, where it goes through various steps in its metabolism and, as seen earlier, initiates the forming of uric acid and fat.
- Food high in refined carbohydrates: Refined carbohydrates directly elevate blood sugar levels, which over time can play a role in insulin resistance. This can result in higher levels of insulin, which inhibits the secretion of uric acid in the kidneys.
- Purine-rich foods: Certain foods should be avoided, or intake reduced if you experience symptoms of high levels of uric acid in your bloodstream. Foods’s rich in purines include meat, especially organ meat such as liver, and red meat such as venison, mutton, veal, and beef. Seafood such as scrimps, scallops, sardines, and anchovies as well as shellfish such as oysters and mussels are high in purines.
- Low purine foods: Most healthy foods are low in purines and cherries contain special pigments (anthocyanins) that can assist in the fight against gout. Coffee is low in purines. Certain fruits are high in vitamin C, which promotes urate removal by the kidneys, such as oranges, grapefruit, strawberries, and pineapples. Low-fat dairy products may promote uric acid excretion, for example low-fat milk and yogurt. Most vegetables are low in purines, for example broccoli, beans, peas, and lentils.
- Foods with moderate amounts of purines: If you are inclined to get gout, some foods should not be eaten in excess, but moderate amounts should be fine to consume daily, for example spinach, asparagus, cauliflower, mushrooms, and oatmeal. Vegetables are also high in healthy fibre and other nutrients.
- Quercetin is a dietary polyphenol, present in red onions, broccoli, apples, berries, cherry tomatoes – it is a pigment that gives colour to many plants – it has potent anti-inflammatory and anti-oxidant properties. In addition, quercetin inhibits the enzyme, xanthine oxidase, which is needed in the final step of uric acid production in the body. It mimics the action of the drug allopurinol, and the suggested daily dosage of quercetin is 500mg.
Conclusion:
It is clear from research findings over the past two decades that high levels of uric acid, mainly from fructose in the diet, are orchestrating a wide variety of adverse health conditions. Uric acid has moved from an innocent bystander, previously only deemed to be involved in gout and kidneys stones, to a central player in metabolic health. Getting uric acid levels down is a way to get back metabolic health. It is strongly suggested that we monitor our uric acid levels annually.
Lifestyle changes can greatly assist with controlling uric acid levels, such as losing weight if you are overweight or obese, following a healthy diet that cuts down on fructose and sugar, getting enough sleep, regular exercising, and drinking lots of water.
References:
Drop Acid. Book by Dr. David Perlmutter. Published 2022 by Little, Brown, Spark. USA. P.324.
Uric acid – blood. Published online and updated 4 February 2022. MedlinePlus. An online health information resource of the National Library of Medicine, part of the National Institutes of Health. USA. (www.medlineplus.gov)
High uric acid level. Published online and reviewed 15 May 2018. Cleveland Clinic. (www.clevelandclinic.org)
High uric acid level. Published 24 June 2020. Mayo Clinic. (www.mayoclinic.org)
Natural ways to reduce uric acid in the body. Published online and reviewed 9 October 2019. Healthline. (www.healthline.com)
All about gout. Published 3 July 2019. Harvard Health Publishing. Harvard Medical School. (www.health.harvard.edu)
Lifestyle changes to reduce the risk of gout attacks. Published 24 April 2019. Harvard Health Publishing. Harvard Medical School. (www.health.harvard.edu)
Fructose metabolism. Article by R.J. Johnson et al from the symposium “Bioinspirational Medicine” JIM Review – Symposium. Journal of Internal Medicine, 2020, 287, pages 252-262. (www.onlinelibray.wiley.com)
Uric acid levels predict future blood pressure and new onset hypertension in the general Japanese population. Published 16 January 2014. Journal of Human Hypertension. 28, pages 529-534 (2014). (www.nature.com)
Review of hyperuricemia as new marker for metabolic syndrome. Published 16 February 2014. Hindawi. (Open access journal publisher.) (www.hindawi.com)
Association between serum uric acid and metabolic syndrome: a cross-sectional study in Bangladeshi adults. Scientific Reports 10, Article number: 7841 (2020). Nature. (www.nature.com)
Interrelationship of uric acid, gout, and metabolic syndrome: focus on hypertension, cardiovascular disease, and insulin resistance. Published 1 January 2018. Journal of Rheumatic Diseases. Official journal of Korean College of Rheumatology (KCR). www.jrd.or.kr)
Examining the connection between gout and metabolic syndrome. Published 2 February 2018. Rheumatology Advisor. (www.rheumatologyadvisor.com)
Uric acid in metabolic syndrome: From an innocent bystander to a central player. Published 15 December 2015. National Centre for Biotechnology Information. US National Library for Medicine. National Institutes of Health. USA. (www.ncbi.nlm.nih.gov)
Physiological functions and pathogenic potential of uric acid: a review. Published14 March 2017. Journal of Advanced Research. Pages 55-61. National Centre for Biotechnology Information. US National Library for Medicine. National Institutes of Health. USA. (www.ncbi.nlm.nih.gov)
Regulation of uric acid metabolism and excretion. Published in International Journal of Cardiology. Volume 213, 15 June 2016, pages 8-14. (www.sciencedirect.com)
What are purines? Updated 28 September 2020. Arthritis-Health. (www.arthritishealth.com)
The effect of uric acid and urinary sodium excretion on hypertension: a nationwide population-based study. Published 27 May 2020. BMC Cardiovascular Disorders. (www.bmccardiovascdisord.biomedcentral.com)
Medical Physiology. A systems approach. (Physiology Handbook). By Hershell Raff, Michael Levitzky, et al. Published 2011. McGraw Hill Medical. P 786.
The shocking science on preventing obesity, diabetes, and chronic disease. 16 February 2022. Podcast interview of Dr David Perlmutter by Dr Mark Hyman. YouTube.
HEALTH INSIGHT
